The issue of genital warts versus herpes is a common one, but there are several distinct differences between the two. Many people confuse genital warts with sores or blisters caused by a herpes infection, but several viruses cause them.
What are genital warts?
Genital warts are caused by the human papillomavirus, also known as HPV. HPV is the most common STD (sexually transmitted disease) in the United States; most people will contract some form of the virus during their lifetime. Like other STDs, HPV is transmitted through intimate skin-to-skin contact, including vaginal, oral, and anal sex.
There are more than 150 types of HPV and the different virus types vary in severity. With most forms of HPV, the virus is asymptomatic and disappears on its own without treatment. However, certain strains of HPV cause genital warts. Other strains can cause cancer of the cervix, penis, mouth/throat, anus, vagina and vulva.
Genital warts caused by HPV appear as small bumps or groups of bumps. They can vary in size and appearance, but are often flesh-colored, raised, and cauliflower-like. They can be removed like warts you would get elsewhere on your body. Genital warts can form on the vulva, penis, scrotum, thighs, lips and around the mouth. Warts can also form on the walls of the vagina, on the cervix and in the mouth or throat, which can be more difficult to spot. Although the warts are usually painless, some people notice itching and bleeding during sex. After you contract HPV, it can take anywhere from six weeks to six months for genital warts to develop (if they develop at all). Sometimes the virus remains dormant for years before genital warts develop.
Other types of HPV can increase the risk of cervical, penile, vulvar, vaginal, anal, and throat/oral cancer. It often takes decades for the virus to cause cancer. These HPV strains do not cause warts; most people don’t know they have the virus until they develop health problems. These types of HPV are transmitted from person to person in the same way as the HPV strains that cause warts.
To prevent transmission of any type of HPV, use condoms or dental dams when you have vaginal, anal, or oral sex. Its use is not as effective at preventing HPV as it is at preventing other STDs, but it does help reduce your chances of becoming infected. Being in a monogamous relationship and knowing your partner’s sexual history also helps reduce the chance of contracting HPV. It is also important to have regular gynecological examinations as part of your sexually active lifestyle. Although a gynecological exam does not typically screen for STDs, a Pap smear can help doctors identify abnormal cells on the cervix that could be caused by HPV. Early detection is crucial: once these cells are recognized, they can be removed to reduce the risk of cervical cancer. Be sure to ask your doctor about other STD tests or cancer screenings.
There is currently no cure for HPV, but the virus often clears up without treatment for people who become infected. Warts that develop can be removed just like warts on other parts of the body. The best thing you can do is prevent yourself from getting HPV by getting vaccinated. The vaccine protects against various types of HPV that cause warts and cancer. Thanks to the HPV vaccine, the number of young people becoming infected is decreasing.
What is herpes?
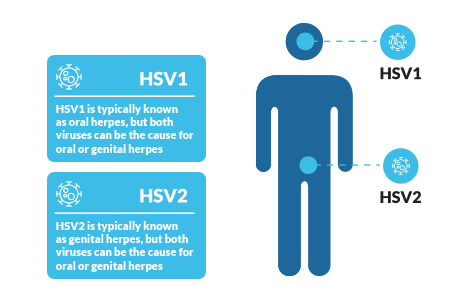
Herpes is an STD caused by one of two viruses: herpes simplex virus type-1 (HSV-1) and herpes simplex virus type-2 (HSV-2). HSV-1 is most commonly known as oral herpes, the virus that can cause cold sores and cold sores on or around the mouth. When people think of genital herpes, they probably think of HSV-2. However, both HSV-1 and HSV-2 can cause oral or genital herpes.
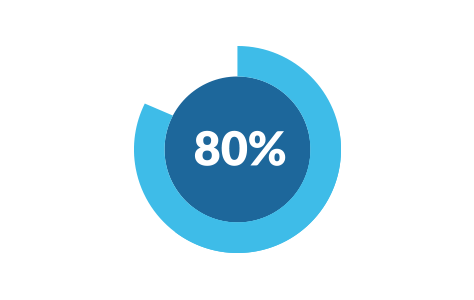
Herpes, like HPV, is common in the United States: the CDC estimates that one in six people in the US has genital herpes and more than half of the US population has oral herpes. Like HPV and other STDs, herpes is spread not only through intimate contact, including vaginal, anal, and oral sex, but also through kissing and any other activity that exposes infected skin to a sensitive area, such as the genitals, mouth, and gums. eyes.
Many people with herpes do not have outbreaks or may not have an outbreak until years after being infected. When they develop, herpes sores look like blisters that then break and turn into painful sores. They can occur on or around the genitals, including the vagina, vulva, cervix, anus, penis, scrotum, buttocks and thighs, as well as on the lips or around the mouth. The virus is most contagious when the sores are present, but you can still get herpes from someone who has the virus but is asymptomatic or has never had an outbreak.
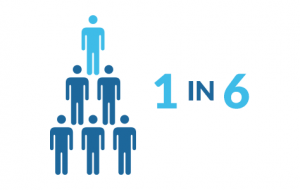
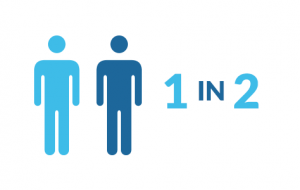
One in six people in the US has genital herpes, and more than half of the US population has oral herpes.
There is no cure for herpes and the virus does not go away. People with herpes have the virus for life. That said, herpes is typically asymptomatic, except during periods when sores develop, also called outbreaks or flare-ups. Many people will experience fewer and fewer symptoms of herpes as time goes on, and outbreaks will typically decrease in severity. There are also medications available to treat symptoms and shorten the duration of outbreaks.
Genital warts versus herpes
Several viruses cause genital warts and herpes. Herpes is not a type of HPV nor is it caused by HPV, and HPV does not cause herpes sores or blisters. People infected with HPV or herpes may have no symptoms. Both viruses are spread through sexual and intimate skin-to-skin contact, so practicing safer sex and limiting the number of sexual partners is critical to preventing the spread of the virus. HPV can even be prevented with a vaccine. There is no cure for HPV or herpes once a person is infected, although treatments are available for both.

